Audet & Partners, LLP is investigating CVS prescription lawsuit claims on behalf of individuals who have purchased prescription medication from pharmacies at either Walgreens or CVS. Information has recently surfaced suggesting that both Walgreens and CVS pharmacies have participated in a fraudulent scheme with pharmacy intermediaries that has resulted in: (1) consumers paying more for medication when using their insurance as opposed to paying cash; and (2) an illegal “clawback” of inflated co-pays which has acted as an improper revenue stream for the pharmacy intermediaries.
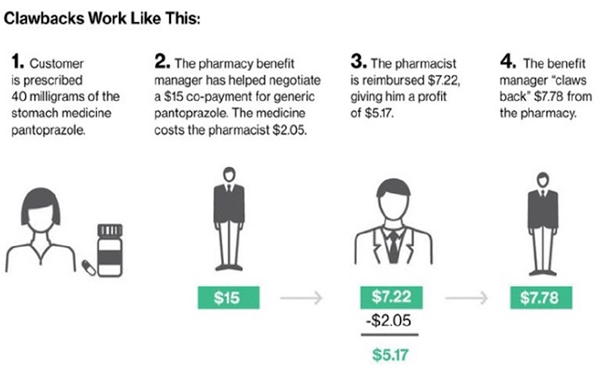
This “clawback” scheme appears to involve third-party intermediaries called Pharmacy Benefit Managers, or “PBMs.” It is suspected that Walgreens and CVS may have entered into contractual arrangements with PBMs pursuant to which the retailers have charged customers more for their copays than generic drugs actually cost, and then pocketed the difference.
Visit our page about pharmaceutical law for more information regarding this practice.
The law firm is no longer accepting clients in this case.